The Anti-Diet: How to be naturally thin by eating what you want.


Learn the 5 principles that naturally thin people do without thinking about it.
Never count calories again
Ditch yo yo dieting
Never overeat
Recognize true hunger
Never do meal plans again
Get answers to the top
30 questions people ask
about intermittent fasting
Unlock tips and help jump start your weight management success
It is a pattern of eating where you restrict the hours that you eat. In my book, and around this site, we refer to this as “eating windows”. You open your eating window when you consume your first meal or snack of the day, and you close your eating window after your last calorie is consumed. There is no magic number of hours each person should remain in their eating window, some people have found that 8 hours work for them, for some it is 6 hours, and others will only eat one meal a day. But the gist of this lifestyle is that you are not restricting the types of food you eat, but instead the hours in which you eat.
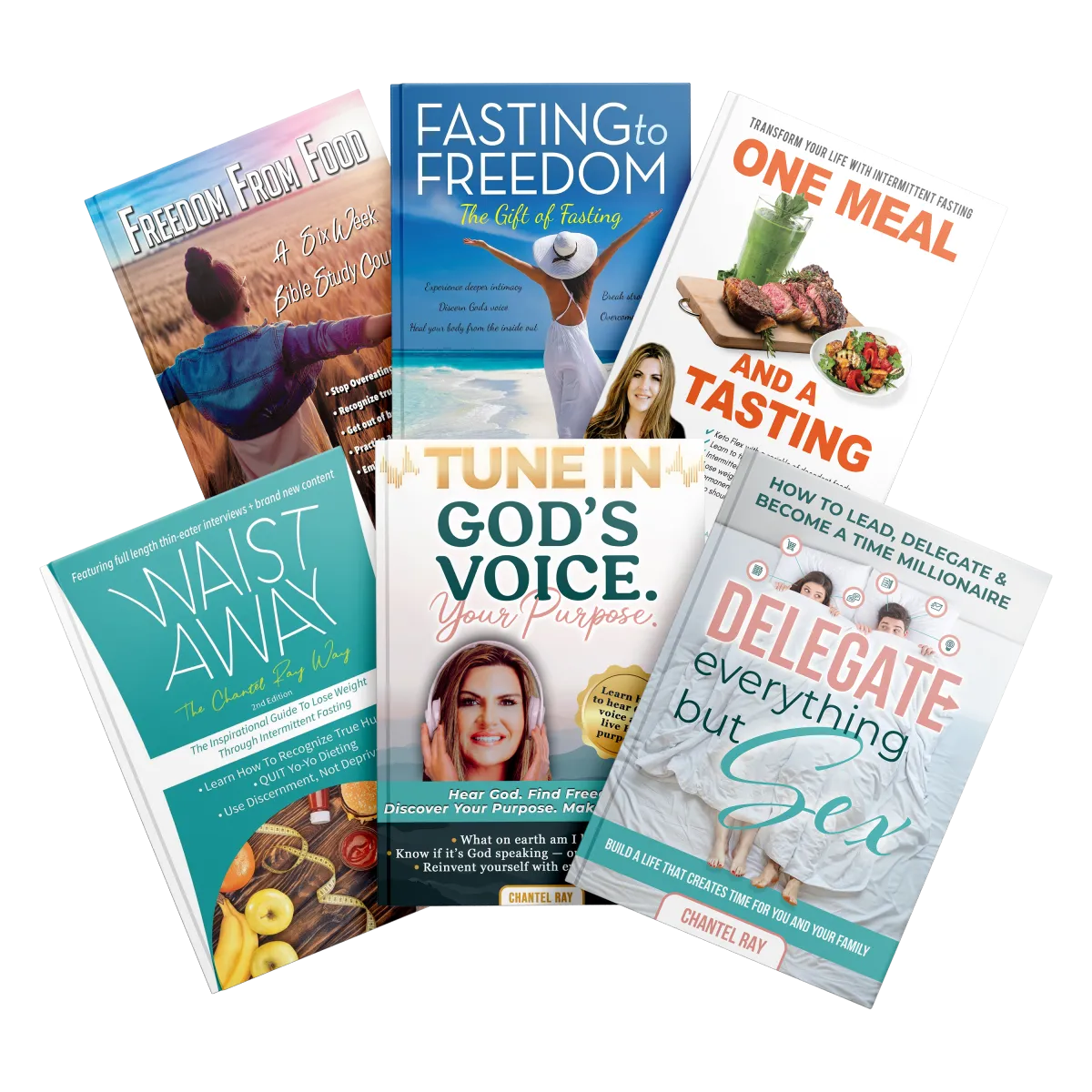
Fasting Books by Chantel Ray
A great starting place for fasting newbies and new tricks for seasoned fasting experts
Each book sold individually or as a bundle.
Get all 4 books in e-book and audio book in one bundle!
Only $39.99
(Workbook is the only one not included in audio book.)
ONE MEAL
AND A
TASTING
When you order Chantel ray's new book "One Meal and a Tasting" on Amazon you will receive FREE entry into the next One Meal and a Tasting Masterclass Session.
Have more questions? Follow the link below to find the top 30 questions about intermittent fasting!
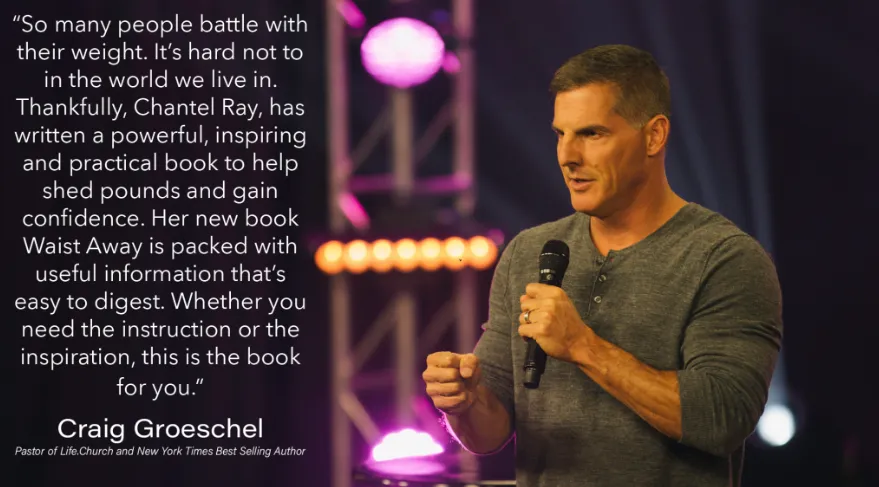
WAIST AWAY
The Chantel Ray Way
The Book That Is Changing So Many Lives
The secrets in this book were first proven to be successful by Chantel Ray herself. She then shared her success with friends and family and became an instant hit. Now her secret is going viral.
Ready to feel in control of food and feel good about your body?
Check out a sneek peak of the EXACT course that I and thousands of my clients used to successfully live a life fueled by freedom instead of living in bondage to food, diets, and weight!
FASTING to FREEDOM
Stop living a mediocre, defeated life! Biblical fasting is a true gift that will allow you to tune in and hear from God, experience supernatural healing, overcome difficult times, receive provision and live in abundance, live under the shelter of God’s protection, and to finally break free from that sin that has you in a choke hold.
Intermittent Fasting (IMF) is a type of scheduled eating plan where you cycle between periods of eating and fasting. The window between meals varies from person to person. Get started with your fasting journey with this FREE intermittent fasting guide!
FREEDOM FROM FOOD
Living a life in bondage to food and skipping from one fad diet to another is exhausting and unfulfilling. God desires a life for you that is free from these strongholds. This 6 week Bible Study uses scripture to teach you to: overcome the temptation of food, avoid gluttony and overeating, understand when your body is truly physically hungry, develop a deeper more meaningful relationship with Christ.
Hear from real people using Chantel's books to accomplish their nutrition and dietary goals.
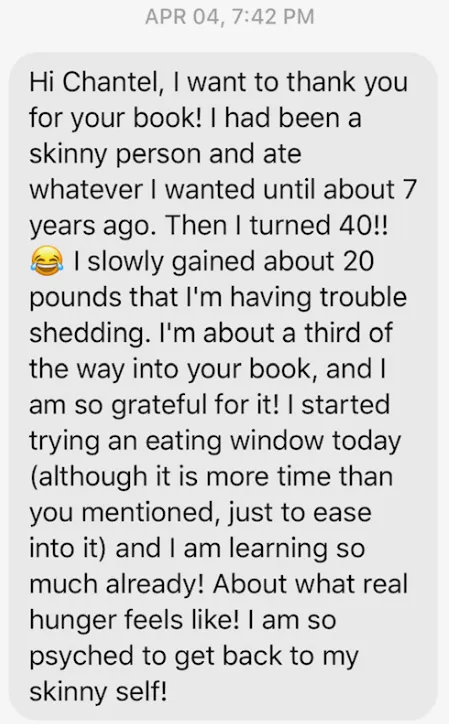
The results you are looking for are attainable. Check out these testimonials from real people looking for real solutions.

HEATHER
I’ve tried many different diets, and I’m so glad to have finally found something that fits my lifestyle. I have been Intermittent Fasting and applying the principles found in this book for 5 months now, and have lost 50 lbs […]

ALLY
I was skeptical when I heard about Intermittent Fasting but decided to give it a try. I have combined Intermittent Fasting with a lower carb lifestyle, and five months later, have lost over 40 lbs and have gained a new perspective […]

LIZ
My name is Liz and I have an incredible testimony that involves this book! At the end of 2015 I incurred an injury at work that would require surgery to rectify the situation. After seeing a specialist I was scheduled to […]
Are you in bondage with food?
Take this 60 second quiz to find out
Do you wish you could break free from the bondage of food and finally feel confident in your own skin?
1. Do you skip pool parties because you don’t want to be seen in your bathing suit
2. Eat an entire pan of brownies after a stressful day at work
3. Try every fad diet under the sun only to lose weight and then gain it all back again
4. Count every calorie that goes into your mouth
5. Overeat in secret and then feel guilt and shame
6. Work out for hours at the gym trying to burn off everything you ate
7. Eat when you’re not even hungry just because you’re bored
8. Hate your body and lack confidence in public


I've lost about 30 pounds by literally interviewing over 1000 women who had been thin their entire lives and learn their secrets. They’ve never been on a diet! I asked them questions about what they did because I believe that people can be thin but still be in bondage to things like:

Food Rules
Excessively working out three times a day or more
Counting Calories
Meal prepping for the whole week
My mission is to teach other people to eat like someone who is naturally thin, and do it effortlessly.
Order the VIDEO COURSE to see what these THIN EATERS EAT!
Learn to lose weight and to become a better you. No more meal plans or fad diets. Learn to not overeat and take control of your body from numerous thin women.
Are you successful in so many other areas of your life but can’t seem to find success when it comes to sustainable weight loss and ending the bondage to food?
I understand because I’ve been where you are and felt what you are feeling.

It's the lessons I learned from my interviews with the thin eaters. They taught me how to:
Free yourself from the bondage of food
Make weight loss and weight management are effortless
I believe that being in a stronghold to food just weighs you down in every other part of your life. It's almost like being an alcoholic….but with food.
You will learn the things that naturally thin people just do instinctively. I believe that maintaining a healthy weight is a skill, and it can be taught, practiced, and mastered. If you're following what these thin eaters are doing, you will learn the basic principles of:
Eating when you're hungry
Stopping when you're full
Not depriving yourself.
Learn to follow the 5 principles that thin people naturally follow.
I am 100% against meal plans and calorie counting. The Chantel Ray Way will never include meal planning or calorie counting because naturally thin eaters never meal plan. They decide what their body is craving, and they eat that!
Understanding
Watch this training video now to learn:
Insight into your attitudes about eating and food
How diets set you up to fail
If food is your "go-to"
Tips to lose weight
To know when you are really hungry
Strategy
Schedule your obligation-free, 10 Minute Strategy Call. We will get to the root of your issues with eating and food and develop a step-by-step plan for success…
We’ll evaluate your current attitudes/habits
when it comes to food/eating.
We’ll look at your goals and challenges
We’ll give you an overview of the Chantel Ray
Way and how it can transform your relationship with food and lead to true sustainable weight loss
Implementation
Get started on your customized plan with the help of a coach. Work with us via one-on-one coaching to transform your attitude, weight, and relationship with food.
Make an investment in your future: Get The Second Edition Book
Join our community: We are passionate and supportive. We’ve been where you are and felt what you’re feeling. We’re here to help motivate you, coach you, and keep you on track: https://www.facebook.com/TheChantelRayWay/
Register for the video course